CPR and DNACPR section live for all users in England, Scotland and Wales
What is CPR and DNACPR
CPR stands for cardiopulmonary resuscitation. It is a treatment that can be given when you stop breathing (respiratory arrest) or your heart stops beating (cardiac arrest).
DNACPR stands for do not attempt cardiopulmonary resuscitation. DNACPR is sometimes called DNAR (do not attempt resuscitation) or DNR (do not resuscitate) but they all refer to the same thing. DNACPR means if your heart or breathing stops your healthcare team will not try to restart it.
Talking about CPR and DNACPR
Depending on the healthcare setting and your health, a General Practitioner, hospital doctor or senior nurse may offer to discuss your thoughts on CPR. There is also a more general desire to talk more openly about people’s wishes on where they want to die and their wishes around the last weeks or months of their lives. You might want to learn about this area before starting a conversation about it with a medical, health or social care professional.
*The information used in MyWishes CPR / DNACPR section was kindly provided by TalkCPR
CPR & DNACPR section on MyWishes
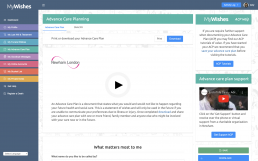
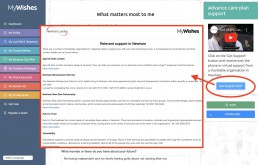
MyWishes now includes CPR and DNACPR information to help educate and empower the general public. This section falls within the Advance Care Planning feature. To learn more register for a free account or login to your account.
Once logged in, visit the Advance Care Plan section and navigate to the relevant section. If you do plan to have a conversation with a healthcare professional about your own CPR and DNACPR wishes we recommend first completing an advance care plan. Once completed, it can be emailed or printed and provided to your GP or anyone involved with your care.

Michael Sobell Hospice Palliative Care Department Mount Vernon Hospital, Gate 3 Northwood HA6 2RN United Kingdom (Map)
- Register and document your wishes for free here
- For all enquires click here
- To learn how MyWishes works click here
Self-empowerment
The best way to ensure that your unique, end of life wishes are adhered to, is to document and discuss them. You are welcome to use MyWishes to assist.
We are a ‘tech for good’ service and everything is free to use. To learn how it works click here.

MyWishes free to use software was developed under the guidance of healthcare, hospice, legal and funeral professionals. Our platform empowers society to make plans for both themselves and those they care about.
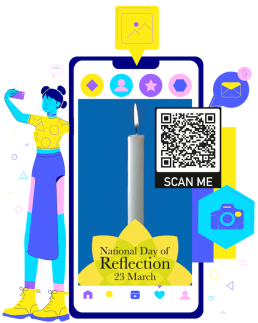
National Day of Reflection - Virtual Candles
We are supporting the National Day of Reflection 2023
The National Day of Reflection will be taking place on the 23rd March for the third consecutive year. Its focus is to unite people who are grieving and allocate a day to remember family, friends, neighbours and colleagues we’ve lost. MyWishes are proud to be an organisation supporting the day and this awareness campaign.
Virtual Candles
We have designed and developed a number of virtual candles. These can be downloaded, streamed and used for free. Our virtual candles are a safe alternative to traditional candles and have been created in different sizes and formats (videos and animated GIFs). The virtual candles were used across on the country and displayed on TV screens, laptops, mobile phones, tablet devices both in 2021 and 2022. They have also displayed in a number of hospices and clinical settings.
Scan the QR Code
If you scan the QR code on the image opposite, a virtual candle will instantly start flickering on the device you are using.
How to use a virtual candle
We recommend thinking about which device you will use to display the candle. We also recommend thinking about the reason for using the virtual candle. These might include remembering a loved one, sharing on social media with an accompanying message or displaying in your home.
If you would like to watch a candle flicker for a one minute reflection, we recommend streaming or downloading a virtual candle in a video format.
If you would like to have a virtual candle flicker continuously on a TV, mobile phone, tablet or on your website, we recommend streaming or downloading a virtual candle in an animated GIF format.
Stream a virtual candle (video)
Click on your favourite virtual candle below. Once opened it will flicker for exactly one minute. The virtual candle videos mirrors the one minute silence being held at 12pm on the 23rd March.
Download a virtual candle (video format)
You can download a candle to the device you are using. To view the virtual candle videos and download your favourite, click on the download button below
Virtual Candle Animated GIFs (for mobile devices and tablets)
We have designed and developed virtual candles and provided them as animated GIFs. Unlike the video virtual candle, these candles will not stop flickering after one minute. These candles will continue to flicker when displayed. The website links (URLs ) shown below each candle can be copied, pasted and used on websites, blogs and social media profiles. If you click on any of the website links shown below, the virtual candle will instantly be displayed in full screen on your mobile device, computer or tablet you are using (these three candles have been optimised for mobile devices)
Animated Gifs versions of the virtual candles can be downloaded and streamed by clicking on the button below. Different sizes (aspect ratios) are also available available for different devices.
Use the virtual candle videos however you want
You might want to display a virtual candle flickering for one minute whilst stood on your doorstep at 8pm on the 23rd March. Alternatively, you might want to position a tablet (iPad, Galaxy Tab, Kindle etc) on a window-ledge and let the animated GIF virtual candle flicker throughout the day .
Virtual candles can also be shared on your favourite social networks by inserting the relevant link into them or uploading the downloaded file.
Displaying a virtual candle on a Wall of Reflection
A Wall of Reflection is a place to share thoughts about loved ones who have died. Walls of Reflection can be created in the home or in a public space. They can be place where people talk with others about loved ones and share memories.
Photos, images, paintings, writings and poems can be attached to a wall. You might also want to display a virtual candle onto a Wall of Reflection. This can be achieved by placing a tablet or mobile phone that displays the candle onto a shelf or by fixing its case to the wall.

Inserting a virtual candle onto a website or blog
Each website and blog is different. The accompanying image highlights a simple way how Wordpress website owners and publishers can insert a virtual candle into a page or post without downloading or embedding it.
Once logged in, simply copy the URL of the virtual candle you would like to use and paste it in the ‘Add media’ section. The candle will flicker automatically and will not require the viewer to press a play button.


MyWishes is the UK’s leading end of life planning software. Our service is free to use and our community document and share their wishes with their loved ones and anyone likely to provide them with care now or at some stage in the future.
“MyWishes will continue to work hard, support society when documenting their wishes and improve understandings around death and bereavement. We are proud to support the National Day of Reflection and understand the importance of this day for the country” – James Norris, MyWishes.

Marie Curie warns that without the right support for people who have been bereaved, the devastation that the pandemic has caused will impact the lives of people for generations. “We need to mark the huge amount of loss we’ve seen this year and show support for everyone who has been bereaved in the most challenging of circumstances. We cannot simply stand by and not recognise the effects the pandemic has had on the bereaved. We know people are in shock, confused, upset, angry and unable to process what has happened. The National Day of Reflection on 23 March gives us a moment to reflect, remember and celebrate the lives of everyone that has died, as well as show our support to family, friends and colleagues who are bereaved during these challenging times – from Covid and other causes.” – Matthew Reed, Marie Curie
Marie Curie, MyWishes, a number of politicians and other supporting organisations are calling on the nation to take a minute to reflect at 12 noon on the National Day of Reflection. To find out more about the National Day of Reflection and how to get involved visit www.mariecurie.org.uk/dayofreflection. If you use social networks, content can be shared on them with the #DayofReflection hashtag.
Scan me
If you use a smart phone (iPhone, Android etc) or a tablet (iPad, Samsung Galaxy, Kindle etc) scan the QR code below with your device. Once scanned a flickering, virtual candle will instantly appear. *Your device will need to have a QR code scanner built into it’s camera for this to work


MyWishes free to use software was developed under the guidance of healthcare, hospice, legal and funeral professionals. Our platforms empowers society to make plans for both themselves and those they care about.
MyWishes Michael Sobell Hospice, Palliative Care Department Mount Vernon Hospital, Gate 3 Northwood HA6 2RN United Kingdom (Map)
- Register and document your wishes for free here
- To learn how MyWishes works click here
Sharing is caring…
Ahead of tomorrow’s National Day of Reflection, you might want to download & display a specially created virtual candle. These are safe, free and can be used by children and adults in a number of ways.
🕯️https://t.co/2UHQieMwm4 🕯️#DayofReflection #techforgood #QRCode #hospice
— MyWishes (@MyWishesApp) March 22, 2022
Contemporary Issues Surrounding Death and Grieving

OxCERPC & Sobell House - Training Day
The training day will focus upon issues surrounding death, dying and grieving in the contemporary setting. Considering different demographic groups, we will look at impacts upon children, upon adolescents and young adults, the impact of digital presence, and social impacts of death & grief. Suitable for: all healthcare and social care professionals eg bereavement counsellors and team members, palliative care professionals, Chaplains/spiritual and pastoral care workers, social workers, art and music therapists, psychologists, GPs, paramedics.
Speakers
James Norris – Founder : MyWishes & Digital Legacy Association
James Norris is the founder of the Digital Legacy Association and MyWishes. James researches and develops end of life technologies, apps and websites. He organises the annual Digital Legacy Conference and publishes regular tutorials helping to empower both professionals and the general public. James runs educational workshops, has consulted various governments and provides thought leadership in digital death, bereavement, technology and the internet.
Dr Jo Wilson BSc (Hons), RGN, DipHSM, BA (Hons), PhD.
Jo is a registered nurse (adult) and team leader of family and bereavement support at Helen and Douglas House (children’s hospice). She is a facilitator of advanced communication skills training and a qualified coach. Prior to her appointment to this role she was Nurse Consultant at the Royal Free Hospitals London NHS Foundation Trust and led three palliative care teams (two hospital teams, and one community), led advance care planning across the trust, and additionally set up and clinically supervised a bereavement service supporting families during and after the COVID-19 pandemic. Her PhD focused on how senior health care professionals recognise dying and negotiate decision-making with patients and their families. She has co-led writing national guidance on care after death and Registered Nurse Verification of Expected Adult Death.
Dr Emily Harrop MBBS BSc DCH FRCPCH PhD Dip Pal Med
Emily has been a Consultant in Paediatric Palliative Care at Helen & Douglas House Hospices since 2010, and the Medical Director since 2019. She is also an Honorary Consultant at Oxford University Hospitals NHS Trust. She is active in research in the field of pain & symptom management and mentors postgraduate research students in the field of palliative medicine. Emily undertook her specialist palliative care training at Great Ormond Street Hospital (including a post graduate diploma in Palliative Medicine); before this she completed a PhD in Neuroscience (Infant Pain) as well as some postgraduate training in Paediatric Clinical Pharmacology. Her other roles include Research Lead of the Association of Paediatric Palliative Medicine (APPM) and joint Chair of the Thames Valley Paediatric Palliative Care Network (TVPCN). Emily has acted as the Co-chair of the WHO Guidelines on the management of chronic pain in children (2020) and the Deputy Chair of the NICE Clinical Guideline Development Group for End-of-Life care in Babies, Children & Young People (NG61). She is currently co-Clinical Lead for CYP Palliative and End of Life Care in NHS South East England.
Emma Jordan – Youth and Transition Worker – Helen & Douglas House Hospice
Emma is a fully qualified and experienced Youth Worker. She has been instrumental in developing and implementing the provision of youth and transition support at Helen and Douglas House and has worked for the organisation caring for young people since 2006. She has been the Youth and Transition Worker for approximately five years.
Emma has worked in various settings throughout her career supporting young people from all backgrounds: residential schools, medical units, residential trips, sailing adventures, youth groups, hospices, and youth clubs.
Emma’s experience and wealth of knowledge gained from working with children and young adults with life-limiting conditions, has informed the nature of the support provided to the young people in her current role. Her other responsibilities include advocating for the young people she supports, being a qualified Young Person Mental Health first aider and being an ‘all-round wellbeing guru’!
Emma is passionate about normalising disability and enabling young people to see beyond societal barriers to achieve the best they can. Her dissertation focused on one important aspect of this: Sexuality and Disability, which is an overlooked area of need. Many young people who have discussed their own experiences over the years voiced that there is still an overwhelming negative societal attitude towards this, and that it needs to be addressed and normalised. Emma has raised the profile of this topic at Helen and Douglas House and has provided training, updated Sexuality Policies, and implemented Care Plans to highlight the importance of this subject.
Rosa Mowles-Van der Gaag – Sibling Team Leader – Helen & Douglas House Hospice
Rosa has been one of the Sibling Team leaders at Helen and Douglas House Children’s hospice since 2017 and works with groups and with children and young people on a one-to-one basis. She has extensive experience of supporting children and families who have experienced the loss of a sibling or have a terminally ill child. Using evidence-based therapeutic approaches she helps them navigate the complex emotions and challenges that arise in the aftermath of a sibling’s death, new diagnosis or life changing event. She focuses on rebuilding family relationships following loss and works with children to process their grief and find generative ways to cope. She has undertaken Media work in her field. Rosa runs experiential seminars to develop staff competencies in working imaginatively with distressed families and children. Rosa has an MA in Educational Psychology and wrote her dissertation on the evaluation of patient services. She also has a Diploma in Family Therapy. Previously she worked on an inpatient CAHMs unit at the Warneford hospital experiencing a range of mental health problems including eating disorders and has extensive experience of working with young people.
Elizabeth Rapa – Senior Post-Doctoral Researcher, Dept Psychiatry, University of Oxford
Louise Dalton – Consultant Clinical Psychologist, Dept Psychiatry, University of Oxford
Others TBC
Course programme
-
Death & Grief in the Digital Age
-
Childrens’ approached to death & dying
-
Grief issues affecting young adults
-
Cultural Differences in approached to death & grieving
Course Aims
-
Consider contemporary issues in death and grief in more detail
-
Appreciate how different factors affect different generations
-
Deepen understanding of the diverse issues faced by people approaching death/experiencing grief
-
Analyse ways in which health & social care professionals can help those to whom they offer care

Michael Sobell Hospice Palliative Care Department Mount Vernon Hospital, Gate 3 Northwood HA6 2RN United Kingdom (Map)
- Register and document your wishes for free here
- For all enquires click here
- To learn how MyWishes works click here
MyWishes free to use software was developed under the guidance of healthcare, hospice, legal and funeral professionals. Our platform empowers society to make plans for both themselves and those they care about.
Advance Care Planning – Three tools for planning ahead
Taking place online on the 28th February 2023 (10:00 – 11:30 GMT)
This event is specifically for Newham charities and organisations who support the general public with care planning activities.
For the past year Newham has been doing some targeted work to raise awareness of advance care planning in the borough. Residents have consistently shared their worries about their end-of-life wishes, particularly about their faith, not being known about. If we are serious about respecting what matters to people and helping them make informed decisions, then advance care planning and the conversations it opens up are really important.
This event will provide an opportunity to hear more about what residents are telling us and to collaboratively develop practical solutions on advance care planning that can be integrated in your day to day practice.

This session will cover:
- Advance care planning what it is and what it’s not
- Service user’s experiences
- Identification and communication tips for having conversations
- Your role in promoting and supporting residents with advance care planning
This webinar will increase your confidence in:
- Understanding advance statements, advance decisions to refuse treatment, and lasting power of attorney in practice
- Understanding advance care planning from Newham residents perspective
- Facilitating conversations with residents around advance care planning
- Your role in informing and supporting residents


Michael Sobell Hospice Palliative Care Department Mount Vernon Hospital, Gate 3 Northwood HA6 2RN United Kingdom (Map)
- Register and document your wishes for free here
- For all enquires click here
- To learn how MyWishes works click here
MyWishes free to use software was developed under the guidance of healthcare, hospice, legal and funeral professionals. Our platform empowers society to make plans for both themselves and those they care about.
LGBT+ History Month - End of Life inequalities

What is LGBT+ History Month
LGBT+ History Month celebrates LGBT+ people in all their diversity, raises awareness and combats prejudice with education.
LGBT+ History Month theme
LGBT+ History Month 2023’s theme celebrates LGBT+ peoples’ contribution to cinema and film from behind the lens.
This includes directors, cinematographers, screen writers, producers, animators, costume designers, special effects, make up artists, lighting directors, musicians, choreographers and beyond.


LGBT+ Inequality in end of life care
In this article we have decided to explore the historical and current inequalities experienced by members of the LGBT+ community at the end of their lives. This can due to a lack of understanding, education and access to information specific to the needs and concerns of LGBT+ individuals.
We have collected and collated snippets of data from three different reports to highlight some of the inequalities experienced within the UK.
The Marie Curie 'Hiding Who I Am' report
In 2016, Marie Curie outlined a number of challenges and concerns held by LGBT+ individuals when engaging with end of life services in the ‘Hiding Who I Am’ report. The report identified six key areas that can lead to LGBT+ inequalities.
1. Anticipating discrimination
2. Complexities of religion and LGBT+ end of life care
3. Assumptions about identity and family structure
4. Varied support networks
5. Unsupported grief and bereavement
6. Increased pressure on LGBT+ carers


Hiding Who I am Report - LGBT+ inequalities within end of life and end of life care
1. Anticipating discrimination
People access palliative care services late or not at all, either because they anticipate stigma or discrimination or they think the service is not for them. Stonewall reports that three in five older gay people are not confident that social care and support services will be able to understand and meet their needs.
2. Complexities of religion and LGBT+ end of life care
Anecdotal evidence suggests that palliative and end of life care services may not always ensure LGBT+ patients and their families have the same spiritual needs addressed at the end of life as any other patient.
3. Assumptions about identity and family structure
Health and social care staff often make assumptions about people’s sexuality or gender identity that have an impact on their experience of palliative and end of life care. Evidence suggests that some clinicians do discriminate on the basis of sexual orientation.
4. Varied support networks:
LGBT+ people at the end of life may choose to be surrounded by close friends and support groups which represent constructed support networks alongside biological ones. LGBT+ people can also feel concerned that their loved ones will not be respected and recognised as next of kin.
5. Unsupported grief and bereavement:
Partners feel isolated or unsupported during bereavement because of their sexuality.
6. Increased pressure on LGBT+ carers:
There is increased pressure on informal carers, because people are accessing palliative and end of life care services late or not at all. LGBT+ people may also experience barriers to palliative care because they are:
– three times more likely to be single
– less likely to have children
– far more likely to be estranged from their birth families (though many LGBT+ people will have alternative family structures in place)
-significantly more likely to experience damaging mental health problems
These factors are likely to lower the chances of stable, ongoing informal care for some LGBT+ people. Informal care, particularly from a partner, plays a vital role in ensuring someone gets access to palliative care. However, further research is needed on how being single influences access to health and social care services at the end of life, and on how adaptable hospice and palliative care services are to alternative friend and family structures.
Accessing healthcare services - The National LGBT Survey
In 2017 the UK government launched the National LGBT+ Survey, the largest of its kind, engaging with over 100,000 recipients. The survey aimed to gather information about the lived experience of LGBT+ people within the United Kingdom. The data below highlights inequalities from those identifying as Transgender.
38% encountered a negative experience because of their gender identity
21% had specific needs were ignored when accessing or trying to access healthcare services
18% said they were subject to inappropriate curiosity
18% avoided treatment for fear of discrimination
Attitudes of health and social care professionals
 Data published by the LGBT+ rights organisation ‘Stonewall’ (2015) highlighted negative attitudes of health and social care professionals towards members of the LGBT+ community. Some of the findings from the report are shown below
Data published by the LGBT+ rights organisation ‘Stonewall’ (2015) highlighted negative attitudes of health and social care professionals towards members of the LGBT+ community. Some of the findings from the report are shown below
58% of health and social care practitioners didn’t consider sexual orientation relevant to a persons health needs
24% of patient-facing staff heard colleagues making negative remarks towards lesbian, gay and bisexual people
20% had heard disparaging remarks about trans people
10% had witnessed a colleague claim someone could be cured of their sexual orientation
Conclusion
Health, social care and palliative care services need to improve the support and service provision provided to the LGBT+ community. Improvements have taken place over recent years however ongoing work, training, review and education needs to take place.
Learn more
- Learn more about LGBT+ Month by visiting https://www.stonewall.org.uk/our-work/campaigns/lgbt-history-month-2023

Self-empowerment
The best way to ensure that your unique, end of life wishes are adhered to, is to document and discuss them. You are welcome to use MyWishes to assist.
We are a ‘tech for good’ service and everything is free to use. To learn how it works click here.


Michael Sobell Hospice Palliative Care Department Mount Vernon Hospital, Gate 3 Northwood HA6 2RN United Kingdom (Map)
- Register and document your wishes for free here
- For all enquires click here
- To learn how MyWishes works click here
MyWishes free to use software was developed under the guidance of healthcare, hospice, legal and funeral professionals. Our platform empowers society to make plans for both themselves and those they care about.
Jonnie Irwin reflects on his digital assets and digital legacy
Jonnie Irwin feature on BBC Morning Live
On Friday, Jonnie Irwin spoke about the importance he places on his ‘Digital Legacy’. Jonnie is a well know public figure familiar to many for presenting ‘A Place in the Sun’ and ‘Escape to the Country’. Last year he received a terminal lung cancer diagnosis and recently reflected on the importance of his digital footprint and the content that will one day help inform his digital legacy.
The feature also included information about MyWishes and how our ‘Digital Will’ service is being used by society to help document, share and safeguard peoples wishes.
Getting your digital affairs in order
- Think about the accounts that you use and where your digital assets are located (online and spread across various electronic devices)
- Backup and share your important assets and information
- Make suitable plans for your online accounts and document your wishes within a Digital Will (also called a Social Media Will)
- Download, sign and share copies of your Digital Will at least one person who you trust
- Document digital assets of a financial value within a Last Will & Testament
- Download, sign and share copies of your Last Will & Testament with at least one person who you trust
- Consider curating your favourite photos and videos and sharing them when you have the capacity to do so
- Consider leaving ‘Goodbye‘ and ‘Scheduled messages‘ for loved ones in the future. This can help bring your digital life to a managed ending
Other news that might be of interest
MyWishes free to use software was developed under the guidance of healthcare, hospice, legal and funeral professionals. Our platform empowers society to make plans for themselves, their possessions and those they care about.

Michael Sobell Hospice Palliative Care Department Mount Vernon Hospital, Gate 3 Northwood HA6 2RN United Kingdom (Map)
- Register and document your wishes for free here
- For all enquires click here
- To learn how MyWishes works click here
Sharing is caring…
Memento Mori Disco

Memento Mori Disco
Memento Mori Disco is an evening party for Palliative Care Congress 2023 attendees.
The Palliative Care Congress 2023 is taking place between the 16th-17th March. Once the first day of the conference has wrapped up, an evening party will take place from 7pm-11pm at the Festival Pub (2 minute walk from the EICC). It will be an informal opportunity for conversations, networking and friendship making to take place.
Music Policy
Palliative Care DJs will be playing music by deceased artists throughout the evening. The music will be chosen be chosen by attendees. Slow songs will be played at the start and the more uptempo songs towards the end.
Request a song using the form below...
Request a song form
Artists already added to the DJs Memento Mori roster range from David Bowie and Queen to Johnny Rotten and 2Pac Shakur. The songs played will celebrate the music and legacy of a diverse and eclectic mix of musicians who have had an impact on the lives of palliative care professionals attending this year’s Congress.



Palliative Care DJs…we need you!
If you work within palliative care, are attending this year’s Congress and also DJ, please get in touch. We would love for you to join other palliative care DJs and perform (we can accommodate whichever setup and controller you are familiar with).
Get in touch by clicking here
Reserve a free ticket now
The party is free to attend but please reserve a ticket in advance for accreditation and entry. The capacity of the venue is 150 people and food will be served until 10pm. If you plan to eat and it’s very busy when you arrive, you might want to eat somewhere else nearby. There isn’t a dress code so conference attire or casual clothing are both fine.

Drink donation / sponsors
This is a not for profit event and is free to attend. If your company or the company you work for would like to buy attendees a few drinks please use the form below. We have capped the bar tab at £1000. If this amount is reached no further sponsors will be able to contribute.
100% of donations will go behind the bar for attendees. Sponsor(s) will receive “thank you” shout outs from the palliative care DJs and the thanks of those attending. The recommended sponsorship amount is £300 – £600. If you are able to provide attendees with drinks, get in touch: https://www.mywishes.co.uk/contact-usget in touch:
About The Palliative Care Congress 2023
The Association for Palliative Medicine of Great Britain and Ireland (APM) hosts the Palliative Care Congress in a different city each year. It attracts over 500 delegates from around the world from a diverse multidisciplinary background. In 2023 the PCC will be bringing Congress to the Edinburgh International Conference Centre (EICC) in Scotland.
To view the full programme click here

MyWishes at PCC 2023
Members of the MyWishes team will be attending and participating in PCC 2023. On Friday James Norris from MyWishes and Professor Mark Taubert a palliative medicine hospital consultant and clinical director at Velindre University NHS Trust will deliver the morning plenary titled ‘Utilising Technology within end-of-life care’.
MyWishes will also be hosting the Memento Mori Disco (as outlined above).

Other news that might be of interest
MyWishes free to use software was developed under the guidance of healthcare, hospice, legal and funeral professionals. Our platform empowers society to make plans for both themselves and those they care about.

Michael Sobell Hospice, Palliative Care Department Mount Vernon Hospital, Gate 3 Northwood HA6 2RN United Kingdom (Map)
- Register and document your wishes for free here
- For all enquires click here
- To learn how MyWishes works click here
Newham Council provides MyWishes for residents
Future health, social care and end of life planning in Newham
Newham residents will benefit from advice and support on ‘End of Life’ planning, thanks to the launch of the Council’s new MyWishes online platform.
MyWishes, commissioned by the Council and tested with residents, can be used to document and share future care and ‘end of life’ choices. The aim is to ensure wishes are understood and followed should a resident lose capacity to make decisions or communicate them. Planning in advance is the best way to help reduce the administrative confusion and stress experienced by loved ones after a death.
"Death remains a taboo subject in society, meaning that many people are uncomfortable with or unsure about discussing what will happen with their affairs after they pass.
This platform will make it far easier for Newham residents to make plans in advance and will relieve much of the stress and difficulty faced by loved ones following a bereavement.”

— Neil Wilson, Cabinet Member for Health and Adult Social Care & Newham Counciler
Empowering residents
MyWishes empowers residents to make ‘Advance Care Plans’ for their health and social care preferences. It also enables residents to document what they would like to happen with their physical property and their digital content (sometimes referred to as ‘digital assets’).
Other features include documenting funeral wishes, writing or recording a self-authored obituary, making plans and leaving goodbye messages to family and friends to be published after death.
After tasks have been completed residents can download and print their documents at home. They can also be emailed to loved ones, there GP and anyone who might be involved with their care in the future. The platform is free and has been adapted to better support residents. It has the support of a number of key local charities operating across Newham.
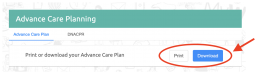

Documents created are downloaded in an accessible and printable PDF format
Making plans in Newham
Registering for a free account
Newham residents can document and share their future wishes by registering for a free account. To do so visit https://app.mywishes.co.uk/register. Once you have registered you will receive a confirmation email from MyWishes with a confirmation link contained within it. Clicking on this link will authenticate your account and email credentials. You will now be able to login to MyWishes using the email and password credentials provided. Please finish setting up your account once registered and enter your postcode. You will now have access to all of the future planning services on MyWishes and no costs will be incurred when using the service.

Receiving support and sharing your wishes
After you have created a document (for example your advance care plan, last will and testament, funeral wishes or your digital will (for your online accounts) download and share the document. Some documents should be signed and witnessed offline. Some documents do not require a signature. An instruction video is provided for each service and further instructions are provided with each document once downloaded or printed.
You might want to share documents with your GP, anyone who might be involved with your care in the future and a friend or family member. We recommend that you also keep a ‘hard copy’ in your home and that you talk about your wishes with at least one person who you trust and your GP should you wish to do so. A number of charities in Newham can be contacted for support when documenting your Advance Care Plan. To view the list of support charities click on the ‘Get Support ACP’ button.
To accompany the platform, the Council has co-designed a Planning Ahead leaflet supporting residents to better understand the options available to them to plan ahead for their future care and for after their death. This is something all of us can do – it is never too early – you do not need to wait until you are unwell or over a certain age.

Editors – Press Release
To download Newham Council’s Press Release and the assets shown for use in publications, websites and blogs please click here
MyWishes free to use software was developed under the guidance of healthcare, hospice, legal and funeral professionals. Our platform empowers society to make plans for both themselves and those they care about.
Other news that might be of interest

Michael Sobell Hospice Palliative Care Department Mount Vernon Hospital, Gate 3 Northwood HA6 2RN United Kingdom (Map)
- Register and document your wishes for free here
- For all enquires click here
- To learn how MyWishes works click here
MyWishes free to use software was developed under the guidance of healthcare, hospice, legal and funeral professionals. Our platform empowers society to make plans for both themselves and those they care about.
Sharing is caring…
The Masterclass in Palliative Care
Introduction
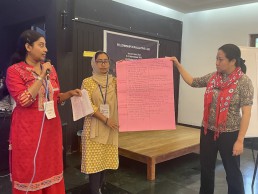
James Norris the founder of MyWishes was invited to attend and participate in an intensive, week long palliative care masterclass. By attending, James hoped to develop his leadership skills and obtain insights into high quality, end of life care services operating across different regions. The following article is an opinion piece written by James about his experiences of the masterclass.
About the Masterclass
The masterclass in Palliative Care took place between 14 November – 18 November 2022 in Kozhikode, Kerala, India. The Masterclass was an advanced interactive learning program in palliative care. The program involved group discussions and faculty-led interactive sessions on the philosophy and practice of palliative care, initiation of supporting platforms and exposure to grassroots-level initiatives in palliative care.
The theme of the program was “Being prepared to lead change”.
Prior to the masterclass I undertook the award winning, ‘Fellowship in Palliative Care‘ programme’. This was developed and delivered by the Institute of Palliative Medicine in Kerala, St Christopher’s Hospice in London, Sanjeevan Palliative Care Project in Pondicherry and the Bangabandhu Sheikh Mujib Medical University in Dhaka. The Fellowship in Palliative Care is a six month programme delivered virtually. The masterclass was a continuation of this learning and conducted at the request of the World Health Organisation (WHO). As part of the masterclass, attendees also contributed to WHO palliative care policy documentation for the South East Asian region.

What happened Masterclass programme schedule
Sessions started at 7:30am and concluded at 7:30pm. There was a strong focus throughout the programme on self-reflection, personal and institutional development. About 60 or so palliative care professionals participated. Some of the sessions were attended by all, others were delivered to better aid the personal development within three specialist fields (doctors, nurses and other palliative care professionals). Further information about the sessions and the full programme can be downloaded (word doc) by clicking here.
With the exception of visiting medical institutes and making visits to people within the local community, everything took place within our newly claimed home. We worked, slept and ate onsite. This along with the intensity of the programme, the duration and the quality of the sessions harnessed a hugely productive educational experience. I slept in one of the ‘male dorms’ with 10 or so other fellows.
We woke up together and had broken conversations whilst we brushed our teeth. We ate breakfast, lunch and dinner side by side. Instead of forging business connections, friendships were made. It was clear that all those attending were passionate about delivering care and improving health ecosystems within our own places of work and counties of residence.
Kerala is the birthplace of ‘Compassionate Communities’. Compassionate Communities is built on a combined ethos of a public health approach to palliative and end of life care and community. ‘Compassion’ was one of the key themes that was explored at a structural and personal level throughout the week.
MyWishes is supporting a recently launched ‘Compassionate Hillingdon’ programme in North West London. This programme is heavily influenced by the Compassionate Communities movement. A number of lessons learned from the masterclass will feed into the future development of the Compassionate Hillingdon programme in the months and years ahead.

The masterclass was the most enjoyable and worthwhile palliative care educational programme I have ever experienced. Working and collaborating alongside others passionate about hospice and palliative care in such an environment has led to friendships and plans for future collaboration that otherwise would not have been possible. Further plans to meet-up with those on the masterclass and invitations to stay in each other’s homes have been both offered and also received.
The feelings that I am now left with about the Masterclass mirrors those of attending Glastonbury festivals. This obscure connection between the two is due to the togetherness, intensity and community created during a relatively short period of time.

Thank you
I would like to thank Dr Suresh Kumar, Professor Heather Richardson, Dr Libby Sallnow, Priyatha Ponnappan, Marie Cooper, Saif Mohammed, Ilyas, the rest of the team, volunteers and all of the fellow masterclass participants for such a memorable and worthwhile experience.
I am certain that the wider, societal and developmental impact of the masterclass in the years to come will be hugely positive and of significance.
The Masterclass in Palliative Care was a masterclass!
About the Author
James Norris is the founder of the MyWishes and the Digital Legacy Association. He also holds a post as a digital research fellow at Michael Sobell Hospice.
As part of James’ work he researches and develops end of life technologies, apps and websites. He organises the annual Digital Legacy Conference and publishes regular tutorials helping to empower both professionals and the general public in areas relating to death and technology.
Document your wishes
MyWishes free to use software was developed under the guidance of healthcare, hospice, legal and funeral professionals. Our platform empowers society to make plans for both themselves and those they care about.
Other news that might be of interest

Michael Sobell Hospice Palliative Care Department Mount Vernon Hospital, Gate 3 Northwood HA6 2RN United Kingdom (Map)
- Register and document your wishes for free here
- For all enquires click here
- To learn how MyWishes works click here
MyWishes free to use software was developed under the guidance of healthcare, hospice, legal and funeral professionals. Our platform empower society to make plans for both themselves and those they care about.
MyWishes accepted onto the West Midlands AHSN's Accelerator programme
WMAHSN Serendip & Accelerator Programme 2022/23.
Overview
We are kickstarting 2023 with some big news… MyWishes are now part of the West Midlands Academic Health Science Network’s (WMAHSN) Serendip & Accelerator Programme 2022/23.
WMAHSN is one of the 15 Academic Health Science Network’s operating across the UK. AHSNs were set up by NHS England in 2013 to operate as the key innovation arm of the NHS.
The 2022/23 health and social care programme will focus on: Transformative Innovation Technology for the Health & Social Care Sector. How can these Digital Tools make better use of data in: Digital Technologies & Data Processing.

What’s next?
Over a 12 month period we will be supported in a number of ways by the WMAHSN team and wider network across the Midlands.
We look forward to building stronger relationships across the West Midlands and improving our offering to all of our users in 2023. The sessions provided in January include a Health Economic training session on the 17th January and a 1:1 benchmarking session.
We would like to say a big “THANK YOU” to WMAHSN for accepting our application.
To learn more about the programme visit: https://bruntwood.co.uk/scitech/business-support/programmes/wmahsn/
Recent news from the MyWishes team...



Michael Sobell Hospice Palliative Care Department Mount Vernon Hospital, Gate 3 Northwood HA6 2RN United Kingdom (Map)
- Register and document your wishes for free here
- For all enquires click here
- To learn how MyWishes works click here
MyWishes free to use software was developed under the guidance of healthcare, hospice, legal and funeral professionals. Our platform empowers society to think about what matters to most and create documents for for their future care, their possessions and those they care about.