Pride Month - LGBTQ+ inequalities with end of life services and end of life care
What is Pride Month?
Pride Month is a yearly event held in June. It celebrates the LGBTQ+ community and commemorates the Stonewall protests that took place in June, 1969. These protests were a catalyst for change and awareness for the LGBTQ+ community and their rights. Since then, Pride has grown and flourished into a series of global events that strides to raise awareness and advocate equality.
Pride comes in all colours, shapes and sizes
There is no ‘one size fits all’ when it comes to celebrating Pride. The main driving force behind Pride month is showing support and compassion by promoting equality, diversity and solidarity within and outside of the LGBTQ+ community. Pride is a celebration of the things that make us unique as well as the things that bring us together.
The MyWishes team fully supports Pride Month and the ways in which it is helping to change attitudes and knock down societal barriers.

Facing Inequality in end of life care
Members of the LGBTQ+ community can experience inequality and discrimination at the end of their lives. This can due to a lack of understanding, education and access to information specific to the needs and concerns of LGBTQ+ individuals.
This Pride Month, the MyWishes team would like to raise awareness of LGBTQ+ inequalities within the end of life sector. We have collected and collated snippets of data from three different reports to highlight some of the inequalities experienced within the UK.

Accessing healthcare services - The National LGBT Survey
In 2017 the UK government launched the National LGBTQ+ Survey, the largest of its kind, engaging with over 100,000 recipients. The survey aimed to gather information about the lived experience of LGBTQ+ people within the United Kingdom. Some data sets within the report found that a range of inequalities exist when ‘accessing healthcare services’. The data below highlights inequalities from those identifying as Transgender.
38% encountered a negative experience because of their gender identity
21% had specific needs were ignored when accessing or trying to access healthcare services
18% said they were subject to inappropriate curiosity
18% avoided treatment for fear of discrimination
The Marie Curie 'Hiding Who I Am' report
In 2016, Marie Curie outlined a number of challenges and concerns held by LGBTQ+ individuals when engaging with end of life services in the ‘Hiding Who I Am’ report. The report identified six key areas that can lead to LGBTQ+ inequalities.
1. Anticipating discrimination
2. Complexities of religion and LGBTQ+ end of life care
3. Assumptions about identity and family structure
4. Varied support networks
5. Unsupported grief and bereavement
6. Increased pressure on LGBTQ+ carers

LGBTQ+ inequalities within end of life and end of life care
1. Anticipating discrimination
People access palliative care services late or not at all, either because they anticipate stigma or discrimination or they think the service is not for them. Stonewall reports that three in five older gay people are not confident that social care and support services will be able to understand and meet their needs.
2. Complexities of religion and LGBTQ+ end of life care
Anecdotal evidence suggests that palliative and end of life care services may not always ensure LGBTQ+ patients and their families have the same spiritual needs addressed at the end of life as any other patient.
3. Assumptions about identity and family structure
Health and social care staff often make assumptions about people’s sexuality or gender identity that have an impact on their experience of palliative and end of life care. Evidence suggests that some clinicians do discriminate on the basis of sexual orientation.
4. Varied support networks:
LGBTQ+ people at the end of life may choose to be surrounded by close friends and support groups which represent constructed support networks alongside biological ones. LGBTQ+ people can also feel concerned that their loved ones will not be respected and recognised as next of kin.
5. Unsupported grief and bereavement:
Partners feel isolated or unsupported during bereavement because of their sexuality.
6. Increased pressure on LGBTQ+ carers:
There is increased pressure on informal carers, because people are accessing palliative and end of life care services late or not at all. LGBTQ+ people may also experience barriers to palliative care because they are:
– three times more likely to be single
– less likely to have children
– far more likely to be estranged from their birth families (though many LGBTQ+ people will have alternative family structures in place)
-significantly more likely to experience damaging mental health problems
These factors are likely to lower the chances of stable, ongoing informal care for some LGBTQ+ people. Informal care, particularly from a partner, plays a vital role in ensuring someone gets access to palliative care. However, further research is needed on how being single influences access to health and social care services at the end of life, and on how adaptable hospice and palliative care services are to alternative family structures.
Attitudes of health and social care professionals
Data published by the LGBTQ+ rights organisation ‘Stonewall’ (2015) displayed attitudes of health and social care professionals towards members of the LGBTQ+ community. Some of the key findings from this report are shown below
58% of health and social care practitioners didn’t consider sexual orientation relevant to a persons health needs
24% of patient-facing staff heard colleagues making negative remarks towards lesbian, gay and bisexual people
20% had heard disparaging remarks about trans people
10% had witnessed a colleague claim someone could be cured of their sexual orientation
Self-empowerment
The best way to ensure that your unique, end of life wishes are adhered to, is to document and discuss them. Documenting preferences around your future health wishes, funeral ceremony and your estate might be appear confusing and difficult. It might not however be as difficult as you first think. Making plans can also help reduce the likelihood of conflicts between friends and family members following your death.
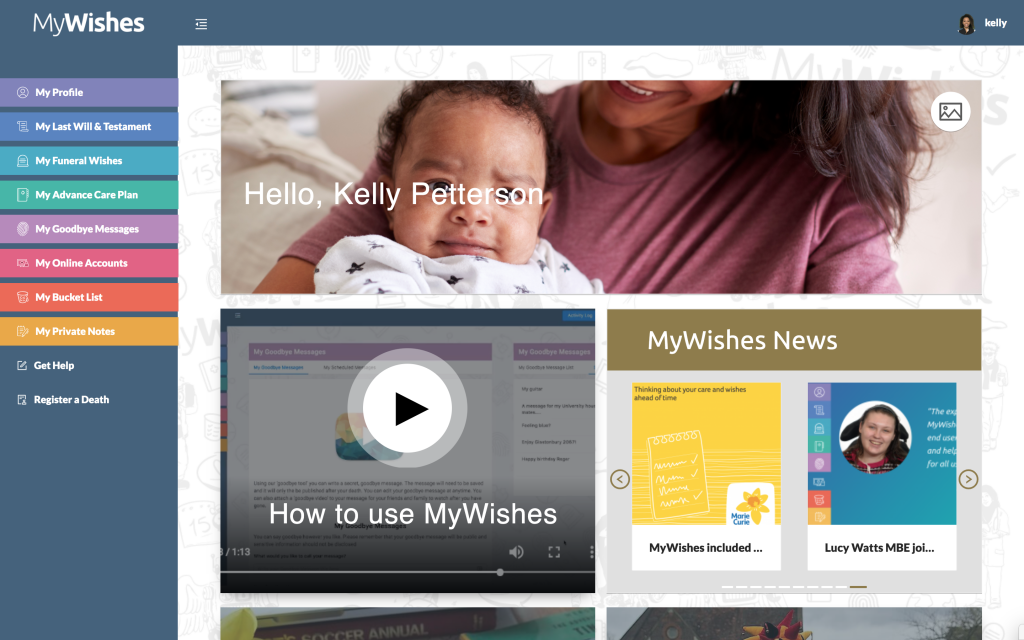
There is no ‘one size fits all’ when it comes to celebrating Pride… There also isn’t a ‘one size fits all’ when it comes to planning for death and dying! MyWishes is a ‘tech for good’ company that tries to be open and available for all. Our end of life planning software is free, you are welcome to join our community and use our platform to help document and share your own wishes. To learn how it works click here.
Conclusion
I’m proud to be living in a time where LGBTQ+ people are not only having their voices heard but are being actively embraced by the community. I am a LGBTQ+ person and researching this area ahead of the publication of this article has been both a poignant and eye-opening experience. I think it is important to note that although the movement towards acceptance and equality is ongoing, the needle is slowly moving in the right direction.
There are a number of issues facing LGBTQ+ individuals at the end of of their life. This stems from a lack of understanding, healthcare service engagement, messaging, societal structures, attitudes, engagement and open communication from care providers.
These important areas need to be addressed in order for end of life care to be provided equally for all. It is my hope that as we keep moving forward and keep pushing for change. Through awareness and advocacy, inequalities around end of life services, death and dying will hopefully become something we look back on and not experience in the future.
– Tom




Get involved this Pride Month
There are many ways you can show support for the LGBT+ community this Pride Month, no gesture is too big or too small. Find more information on how you can get involved and upcoming events in
- London by clicking here
- Brighton by clicking here
- Manchester by clicking here
- Liverpool by clicking here
- Birmingham by clicking here

MyWishes free to use software was developed under the guidance of healthcare, hospice, legal and funeral professionals. Our platforms empowers society to make plans for both themselves and those they care about.
Further reading
- National LGBT Survey: Summary report (publishing.service.gov.uk)
- The reality of end of life care for LGBT people (mariecurie.org.uk)
- Unhealthy Attitudes (2015) (stonewall.org.uk)
- I Just want to be me (Hospice UK, 2022)
- MyWishes leaflet (free to download and use)
- Getting your digital affairs in order
- Why you need a Social Media Will


Michael Sobell Hospice Palliative Care Department Mount Vernon Hospital, Gate 3 Northwood HA6 2RN United Kingdom (Map)
- Register and document your wishes for free here
- For all enquires click here
- To learn how MyWishes works click here
Sharing is caring…
EOLP Annual Conference 2022
EOLP Conference of Care 2022
We are excited to announce that we will be participating in this year’s annual EOLP conference taking place on Thursday 29th September 2022 at the Best Western Forest Hills Hotel, Cheshire.
This year’s theme will explore some of the paradoxes presented within the Lancet Commission report on the ‘Value of Death: bringing death back into life’ (pub. Jan 2022) while reflecting on current practice and approaches. The Value of Death: bringing death back into life, based on the recommendations of the Lancet Commission report, The Value of Death: bringing death back into life (.pdf) which sets out five principles of a realistic utopia, a new vision of how death and dying could be.


James (the founder of MyWishes) will be providing two workshops titled ‘How MyWishes is normalising end of life planning’. He will demonstrate how user-centred design principles and person-centred care can take place online. It will allow participants to reflect on the plans that they have made for themselves from both a physical and digital perspective. He will ask participants to then reflect on their own personal and professional practices and think about how they might evoke change within this space within their hospice, charity or place of work.
The workshop will conclude with the sharing of resources, information and best practice. The objective of the workshop is to empower participants to better support the communities they serve. The full conference programme can be found below
EOLP Conference Agenda
Time
Session
8:45
Registration desk is open
9:15
Welcome and housekeeping
Dr Lynne Partington, Project Coordinator and Education Advisor, The End of Life Partnership
9:20
Chair’s opening comments
Salli Jeynes, CEO, The End of Life Partnership
9:35
The Lancet Commission on the Value of
Death: paradox, systems and the future
Dr Libby Sallnow, Honorary Senior Clinical Lecturer, Marie Curie Palliative Care Research Group, University College London
10:10
Gender, networks and stories
Dr Ros Taylor MBE, Medical Director
Michael Sobell Hospice and Harlington Hospice
10:45
A carer’s lived experience
Sandra Smith
11:00
A summary of the morning so far and moving onto workshops
Salli Jeynes/Lynne Partington
11:10
Coffee break
11:45
Workshop 1 (Choice of 1 of 5)
How MyWishes is modernising end of life planning
James Norris, Founder of the Digital Legacy Association Digital Legacy Conference and MyWishes
Improving Equitable Access to Palliative
and End of Life Care for Inequality
Groups
Heidi McIntyre, Homeless Palliative Care
Coordinator, St. Ann’s Hospice and Siobhan Kenyon, Learning Disability & LGBT Palliative Care Coordinator, St Ann’s Hospice
Schwartz Round: Words don’t come easy
anymore. Using Schwartz Rounds to
support workforce resilience and
compassion
Amy Sinacola, Schwartz Round Mentor, The Point of Care Foundation and Annamarie Ratcliffe Macmillan Head of Service & Practice Development (East Locality), The End of Life Partnership with Alison Clifford and Jenny Casson
Building an experience based service
through the effective use of data
Dave Reed MBE, Project Manager and Kay Howard, Macmillan Palliative Care Clinical Nurse Specialist, Palliative and End of Life Care Programme, NHS Lincolnshire CCG
Relaunch of the Blue Booklet.
Anticipatory medication at end of life:
The choices and the challenges
Lorraine Dunne, Locality Coordinator, The End of Life Partnership
12:45
Lunch
13:45
Workshop 2 (Choice of 1 of 5) As above
As above
14:50
Tea break
15:20
Conversations about death
The Frodsham Players
15:45
Achieving a realistic utopia
Dr Karen Groves MBE, Medical & Education Director, Queenscourt Hospice; Honorary Clinical Professor, Edge Hill University
16:15
Chair’s closing comments
Salli Jeynes, CEO, The End of Life Partnership
16:20
Close
Other events we are involved with…
MyWishes free to use software was developed under the guidance of healthcare, hospice, legal and funeral professionals. Our platforms empowers society to make plans for both themselves and those they care about.

Michael Sobell Hospice Palliative Care Department Mount Vernon Hospital, Gate 3 Northwood HA6 2RN United Kingdom (Map)
- Register and document your wishes for free here
- For all enquires click here
- To learn how MyWishes works click here